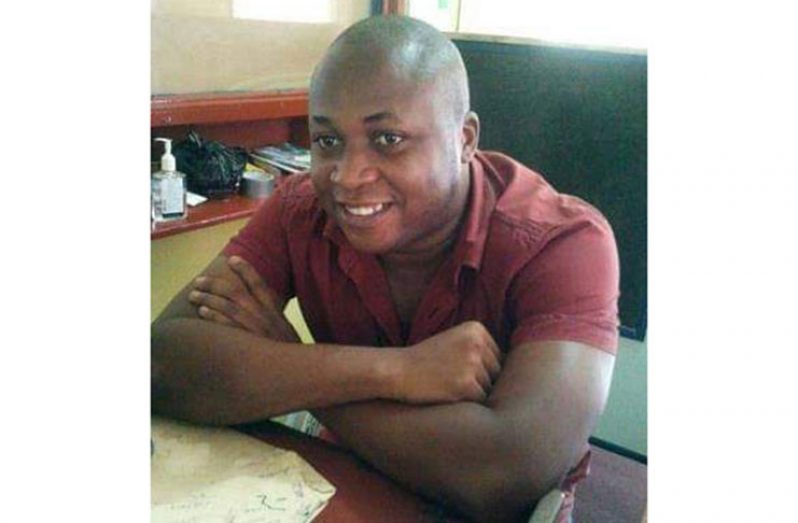
-recovered COVID-19 patient recounts battle with the disease
IT started with just an itch in the throat and ended with his kidney failing, but Kwasi Lewis survived and is here to tell the story of how he survived the battle against the deadly Novel Coronavirus (COVID-19) disease.
About five weeks ago, Lewis woke up, thinking it would be another routine day, under quarantine – as the rest of the country – but it was far from that, as it was the first day he experienced a symptom of the COVID-19 disease, a sore throat.
Common knowledge over the past four months has been the symptoms of COVID-19, which according to the World Health Organisation (WHO) include fever, dry cough, tiredness, aches and pains, sore throat, diarrhoea, headache and shortness of breath, among other things.
Note, even prior to COVID-19, a sore throat was and remains a common symptom of the flu or the common cold, conditions which Guyanese usually treat with traditional home remedies. Not assuming the worst, Lewis though he was just “under the weather.”
“I started feeling an itching in my throat then it quickly escalated in a few days…I got a fever, I started coughing, I had severe diarrhoea and I started to lose energy,” said Lewis in a telephone interview with the Guyana Chronicle.
Knowing that it was definitely not the common cold or the flu, Lewis quickly distanced himself from his family and made contact with the medical professionals at the Georgetown Public Hospital Corporation (GPHC), who advised him what to do.
Based on guidance and advice from the health workers at GPHC, Lewis made his way to the hospital, where he was screened and tested for the disease. It was no surprise that the test was positive, but what baffled him was where he could have contracted the disease from.
The survivor said he was very careful, especially after news broke about the disease reaching Guyana. He said he adhered to all the existing measures, wore his mask and used sanitisers, but still ended up at the mercy of COVID-19.
The disease didn’t show its severe form at the start, and according to reliable sources from GPHC, Lewis’ condition had become less severe in a matter of days, making him stable. Considering his stable condition, hospital officials decided that the patient should be transferred to the West Demerara Regional Hospital, another COVID-19 facility, which is used for the isolation and treatment of stable patients.
Like every smooth road, there is bound to be a pothole or two along the way, and Lewis had hit that “pothole” a few days after been isolated at the West Demerara Hospital. Hospital sources told the Chronicle that the patient started to develop severe complications, which persisted and got worse.
His deteriorating health caused concerns at the West Demerara Hospital, to the point where they decided that he had to be transferred back to GPHC.
“I got really sick and at GPHC, they discovered that I had Kidney failure…they don’t know if is the coronavirus caused it because they said it could have happened before but the corona rile it up,” said Lewis, who said he had no known underlying condition, prior to contracting COVID-19.
According to an international organisation called the Urology Care Foundation, the kidneys are two bean-shaped organs, each about the size of a fist. They are found in your back on either side of the spine. Healthy kidneys clean waste products from the blood by making urine. They also balance the amount of certain elements in your blood (such as sodium, potassium, and calcium), and make hormones that control blood pressure and red blood cells.
And, according to the organisation, kidney (renal) failure is when kidneys don’t work as well as they should, meaning they cannot perform the normal functions.
In further recounting his harrowing experience, which was exacerbated by renal failure, he said: “There were times in the ICU I thought it was the end because I was told if I don’t get a dialysis for my kidney that could be it.”
In order to save Lewis’ life, GPHC had to act quickly and establish a special dialysis unit to treat COVID-19 patients because the risk of spreading the disease would have been high if they had taken him to the normal facility.
The administration of the hospital, as was reported by this publication, managed to make the necessary adjustment and has since established a temporary dialysis unit, the very unit that saved Lewis’ life. He was treated and discharged from the COVID-19 Intensive Care Unit (ICU) last week.
“The team at GPHC is the best, they did their best and I am grateful because I am here today,” said Lewis, adding that while he was grateful for life, he was most thankful because no member of his family contracted the disease.
While the delivery of healthcare played a big part in ensuring that he survived, Lewis said he kept the faith and encouraged himself to get better, every day.
WILL NEVER FORGET
Although Lewis was tested twice and cleared of COVID-19, he continues to battle the effects caused by kidney failure.
“This is a battle I will never forget…I am still battling the kidney injury and I have to go to the hospital daily, but I have to keep the faith… I fought many battles and I have to fight this one too,” said the COVID-19 survivor.
Today, he remains a living example of the effects of COVID-19 and he urged persons to adhere to the preventative measure because COVID-19 is real and dangerous.
Lewis is among 43 persons locally, who have successfully battled the COVID-19 disease and have been medically cleared by health authorities.
This, however, does not change the fact that the COVID-19 disease has proven to be a “real killer,” especially in cases involving persons who have co-morbidities. Ten persons have lost their lives to the disease, in Guyana.
And according to a report from the Guyana Chronicle, most of the persons who died had co-morbidities. In medicine, comorbidity is defined as the presence of one or more additional conditions co-occurring with a primary condition; in the countable sense of the term, a comorbidity is each additional condition.
The World Health Organisation (WHO) had said that 81 per cent of persons who contract COVID-19, will have mild symptoms, while 14 per cent will have severe symptoms and five per cent will need intensive care.
“Most of the people who passed, have [sic] co-morbidities…some had diabetes, hypertension, asthma and one of them even had severe pneumonia, which, without COVID, can also cause death…these, coupled with the complications related to COVID-19, can be dangerous,” said Head of the Department of Internal Medicine at GPHC, Dr. Genellys Camps, during an exclusive interview with the Guyana Chronicle.
In Guyana, as part of strengthening the systems in place to reduce the spread of the virus, the Public Health Ministry had said that alternative arrangements were created for patients who are immuno-compromised, to collect their medication without putting themselves at further risk.
These patients include persons who have cancer, HIV, tuberculosis, sickle cell and other diseases. They were also advised to take extra precautions in order to safeguard themselves.



.jpg)