— survivor tells of fight to overcome depression, suicidal thoughts
STRUGGLING to cope with the realities of life, Samantha Sheoprashad had made several attempts on her life after falling into a severe state of depression but it was the constant message of hope that kept her head above the rough waters.

Today, she is one of the 2017 Queen’s Young Leaders championing the cause for mental health issues to be placed on the front burner.
As she walked down memory lane, the 27-year-old Enterprise, East Coast Demerara (ECD), web designer said had it not been for the unwavering support of her friends, lecturers, counsellors and psychologist, she would not have been here to tell the story.
Growing up in Enterprise with her extended family, Samantha said at an early age she was confined to the social and cultural traditions of society – a society back then that placed little emphasis on advanced education for girls and women.
A society that taught girls and women that marriage was the best option and they were best placed in the home.
Determined to break the barriers set by her village, Samantha at the age of 21 opted to attend the University of Guyana, Turkeyen Campus.
“My family didn’t afford me the opportunity to go to the university, so I had to battle that on my own,” she said.
Samantha started to read for her degree in computer science at a time when she was battling with severe depression and symptoms associated with mild schizophrenia.
According to the World Health Organisation (WHO), schizophrenia, like depression is a mental disorder, however, it is characterised by profound disruptions in thinking, affecting language, perception and the sense of self.
Ignorant of the mental illness, Samantha was categorised by some as a demonic person.
“Religious bodies who saw my dilemma thought that I was possessed and they would have prayed. They did more than six years of prayers and fasting but nothing ever stopped it,” she recalled.
Her battle with the mental disorders was further compounded by the abusive relationship her parents shared and her inability to secure a job to sustain herself while attending the university.

“The painful part of it was not being able to have a job and study…you go to so many different interviews, you are not qualified because you are young, you are not qualified because you don’t have this, you are not qualified because you are studying, nobody wants anybody who is studying,” the Queens Young Leader said as she spoke passionately.
Overwhelmed by her circumstances, Samantha decided to quit UG and end her life but was stopped in process by Narendra Nauth – a young man who she had grown close to while studying the same programme at the university.
For hours, he spoke her out of it, but it was not long after that she made other attempts.
Realising that she needed professional help, Narendra took her to an American Psychologist, Dr. Eton Simon.
“From there on I started to heal I started to recover,” the young lady said. She was 23 when the healing process started. She also had counselling sessions at the university.
SUPPORT FROM COLLEAGUES
While away from counselling sessions, Samantha received much-needed support from her

colleagues and the lecturers at the university.
“Both Malcom Williams and Eldon Marks (my lecturers) coached me through that period of time and provided that support relentlessly… Malcom was more of a logical person, Eldon came on with a spiritual point of view, and he came on with the meditative aspect. He would be like Sam, meditate on something that would bring you peace,” she recalled.
Even as she continues to heal, Samantha launched the Enterprise Youth Development Group as she created that safe space for young people to express themselves, in particular those dealing with depression and suicidal thoughts.
“Talking helps and it is important for us to create that space where young people can express themselves, where they can be encourage and receive the guidance they need.”
It was that space and support that a 42-year-old taxi driver in Central Georgetown may not have had, that caused him to end his life after years of battling with alcohol abuse, his foster daughter, who requested anonymity, said as she cried silently.
November, 2017 will mark one year since the father of four took his life, but the pain of his passing remains fresh in the hearts of many.
“Sometimes I think, maybe if I had reached out to him, maybe if I had given him a chance to tell his side of the story, he would have been here with us today. I regret not doing that,” she said.
In addition to alcohol abuse, the taxi driver was having domestic problems with his wife over his fear that she was being unfaithful.
Mary (not her real name) said her foster father, who was providing for her since she was five, committed suicide 11 years ago.
“He heard that if anyone is found committing the act and they survive they will be charged and placed before the court. He didn’t want to be charged and placed before the court so he left and never got professional counselling or his treatment,” Mary recalled. Today, she is calling for the decriminalisation of suicide, contended that her foster father could have gotten the professional help he needed if he was not fearful that he would have been placed behind bars.
While mental illnesses such as depression and alcohol abuse are not the only reasons why people attempt to commit suicide or commit suicide, they are some of the primary reasons, especially in low and middle-income countries.
On the basis that suicide is a serious public health concern, Pan American Health Organisation/World Health Organisation (PAHO/WHO) representative, Dr. William Adu-Krow continues to call for the decriminalisation of suicide in Guyana.
ARCHAIC LAW
During a parliamentary confab last July, Dr. Adu-Krow said there is an urgent need for legislative changes to be made as he alluded to the Criminal Law Offences Act Cap.8:01, the Summary Jurisdiction Offences Act Cap. 8:02 and the Pesticides and Toxic Chemicals Control Act Cap, 68:09. Reference was also made to the Customs Act, the Food and Drugs Act and the Mental Hospital Ordinance Cap. 140.
Pointing to Section 95 of the Criminal Law Offences Act, Cap. 8:01, he concluded that the legislation would only fuel more suicides. According to that section, “everyone who aids or abets any person in the commission of suicide shall be guilty of felony and liable to imprisonment for life”.
It is belief that if a person escapes prosecution, that person is encouraged to commit suicide.
Section 96 criminalises the act, and creates provision for imprisonment. “Everyone who attempts to commit suicide shall be guilty of a misdemeanor and liable to imprisonment for two years,” Dr. Adu-Krow said while quoting the law.
But Director of the Mental Health Unit, Dr. Util Richmond-Thomas, during an exclusive interview with Guyana Chronicle, said while the “law is on the books, it is not enforced”.
According to her, the decriminalisation of suicide is not on the front burner for Guyana currently, stating that it may be pursued in the future.
WHO states that every year close to 800, 000 people take their own life, noting that there are many more people who attempt suicide.
Guyana, according to WHO, in 2015 had the second highest suicide rate in the world after Sri Lanka with a rate of 30.6 deaths per 100, 000. Sri Lanka has the highest rate with 34.6 deaths per 100, 000. Recent data shows that Guyana has the fourth highest suicide rate in the world with an estimated 29.0 per 100,000
Using 2014 as a baseline with a suicide rate of 34.7 deaths per 100, 000, the Public Health Ministry in its compilation of the National Mental Health Action Plan 2015-2020 with support from PAHO/WHO, had set a target of 25 per 100, 000 for 2017, and less than 20 deaths per 100, 000 for 2020. It is unclear whether Guyana will meet that target.
PROGRESS
But Minister within the Ministry of Public Health, Dr. Karen Cummings said the country has been making progress, pointing that in the past it had the alarming suicide rate of 44.2 deaths per 100,000 people.
The statistics in 2012 have shown that suicide was the leading cause of death among young people aged 15-44, and the second leading cause of death among the 20-24 age group.
Females attempted suicide more frequently than their male counterparts at a ratio of 3:1; East Indians had accounted for 50 per cent of the cases whereas Afro-Guyanese had accounted for 26 per cent of cases, the minister reported as she addressed the parliamentary confab in July.
The common risk factors identified were acute emotional distress and depression (37 per cent), accessibility to lethal substances such as herbicides and pesticides (64 per cent), alcohol and drug use (32 per cent) and family dysfunction (34 per cent).
According to her, the coalition government has been taking critical steps to arrest the situation, pointing to the work of a multi-disciplinary team formed by President David Granger to address the issue.
The Ministries of Education, Social Protection, Agriculture, Indigenous Communities and Public Security make up the National Task Force which covers four strategic areas: (1) Risk Factors Reduction, Health Promotion and Prevention; (2) Reduction of Access to the Means of Suicide; (3) Health Systems response to Suicide Behaviour; and (4) Surveillance and Research.
Though not providing Guyana Chronicle with current stats, the Director of the Mental Health Unit said that the numbers were dropping.
“By next year we will have a comprehensive figure out,” she said.
However, in July, Dr. Richmond-Thomas had disclosed that for the period January to May 2017, the Guyana Police Force (GPF) recorded 92 cases of suicide while the Ministry of Public Health recorded 59 cases.
But she said the ministry was still in the process of collecting data from health facilities countrywide. In 2016, she recalled that there were 169 cases. The police at the time had reported 99 cases. Most of the deaths occurred among persons between the ages of 15- 29, most of whom were male of Indian descent.
RED AREAS
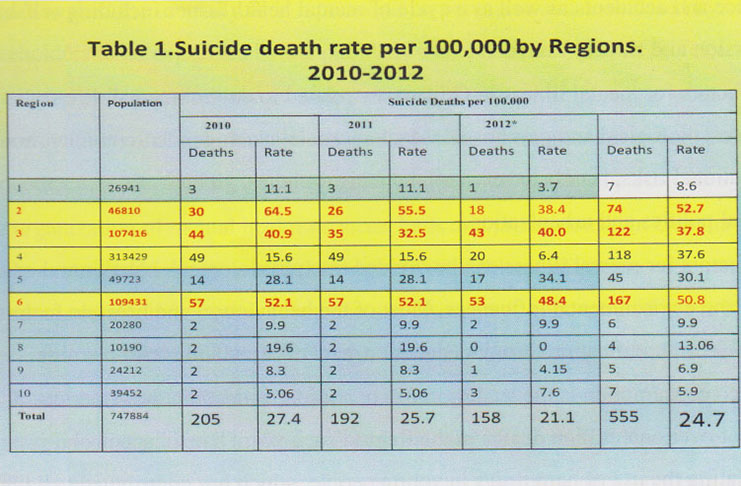
Despite faced with a shortage of social workers and psychologists, Dr. Richmond-Thomas said the Mental Health Unit is placing significant attention on the problematic areas – Regions Two, Three and Six.
It was noted that in Regions Three and Six, many persons are battling alcoholism, depression and dysfunctional families.
“Unavailability of jobs and economic stresses are major problems along with relationship issues,” she added.
Through the Mental Health Unit, Dr. Richmond-Thomas said persons who have been detected with suicidal tendencies are being thought how to cope with the issues facing them.
Currently, the unit, which was formed in May 2016, has six psychologist, eight social workers, and two health education officers; however, one of the social worker was transferred to Region Six while a psychologist has been transferred to Region Two.
TRAINING DOCTORS
“One of the major strategies of the Mental Health Unit has been to train doctors in mental health conditions. So we have trained doctors in Regions Three, Four and Six,” she posited, while noting that some 60 doctors have been trained to manage mental illnesses.
Training of these doctors is critical given the shortage of psychologists and psychiatrists in the country. Currently, there are vacancies within the unit for six psychologists and eight social workers, but the director believes that there should be social workers at every health facility in the country.
“All are non-specialist doctors. Not all of these doctors are at the hospitals; a lot of them are at the health centres. Community mental health [is a work in progress], if you suspect that your family has mental health problems, you can go into the health centres and you will find a doctor there who can manage your issue,” she added.
The training which is in keeping with the Plan of Action is expected to be for a period of two years.
In addition to the training, the unit is preparing proposal to be submitted to the Public Health Ministry which will teach problem-solving skills and refusal skills to young people, dealing specifically with the alcohol abuse.
The unit is also working with the Pesticides and Toxic Chemicals Control Board to ensure pesticides and chemicals are safely transported and stored.
THE Guyana President Association (GPA) has joined other government and non-governmental organisations in the fight against suicide. For the GPA, it is to ensure that journalists and reporters report responsibly on cases of suicide.
Subsequent to the 2016 PAHO/WHO media workshop on suicide, GPA President, Neil Marks said there has been noticeable improvement. According to him, many reporters are no longer giving detailed information in their reports such as the methods used to commit suicide; however, there have been lapses.
“There are still occasions where those who are not trained or educated still carry those things but especially the methods of suicide we have tried to get people not to report on those,” he explained. Cognisant of the situation, Marks said the GPA is constantly policing reporters to ensure they report responsibly on this scourge.
The Public Health Ministry has noted that it is working in conjunction with the Guyana Police Force to keep the Guyana Inter-agency Suicide Prevention Help Line operational.
A call to the help line – 223-0818 – proved that it is working. Answering on the other end of the line was Sherry Maison. After informing Maison that it was a journalist on the line and the purpose of the call, she explained some days are busier than others.
“People come with different problems. Some people just want to talk. Sometimes we have to put them onto the counsellors. We are not fully trained, we are taught the basics but we try our best to help,” she posited.
Domestic problems, alcoholism, drug abuse, spiritual issues, relationship issues and family issues are among the common issues callers have.
“Some would have called after consuming tablets and we would make arrangements to get them to the nearest hospital. They are examined and counsellors are assigned to them,” she further explained.
Callers, according to Maison, most times range from 14-75. The help lines are operational 24/7 and include 223-0818, 223-0009, 223-0001, 600-7896 and 623-4444. If you are feeling depressed or troubling from other mental illness, remember there is someone on the other end of the line waiting to speak to you. Break the silence! Take a minute, save your life, it is not too late.












