INFECTIONS caused by Candida species of fungus comprise one of the most common oral disease conditions encountered in the practice of dentistry. As a dentist having to work with patients suffering from a variety of medical conditions including HIV/AIDS, I have encountered this situation frequently. In the majority of cases, the disease may clinically present itself in several different forms. It is mainly observed as white, soft plaques overlying areas of redness on the mucosa (lining) which are removed easily, possibly showing pinpoint areas of ulceration sores. In infants, it is commonly referred to as thrush.
 When clinical Candidosis emerges, it can result from a variety of predisposing or associated factors. These factors include but are not limited to age extremes, malnourishment, metabolic diseases, concurrent infection with other harmful germs, antibiotic treatment, HIV infections and radio therapy. Candida can be found in the mouth and anal region of newborns at a rate of approximately 40 per cent, which correlates well with vaginal carriage of the mother at the time of birth. However, the disease affects 4 to 10 per cent. These infections appear as milky white curd like plaques which are easily removed by digital rubbing and are generally evident three to seven days after birth.
When clinical Candidosis emerges, it can result from a variety of predisposing or associated factors. These factors include but are not limited to age extremes, malnourishment, metabolic diseases, concurrent infection with other harmful germs, antibiotic treatment, HIV infections and radio therapy. Candida can be found in the mouth and anal region of newborns at a rate of approximately 40 per cent, which correlates well with vaginal carriage of the mother at the time of birth. However, the disease affects 4 to 10 per cent. These infections appear as milky white curd like plaques which are easily removed by digital rubbing and are generally evident three to seven days after birth.
With the increase in age and a corresponding increase in the diversity of the germs that naturally inhabit the mouth, there appears a corresponding reduction in the incidence of the signs and symptoms of Candidosis. This may be the result of increasing environmental competition in the oral cavity as well as the child’s developing competence to fight off infections.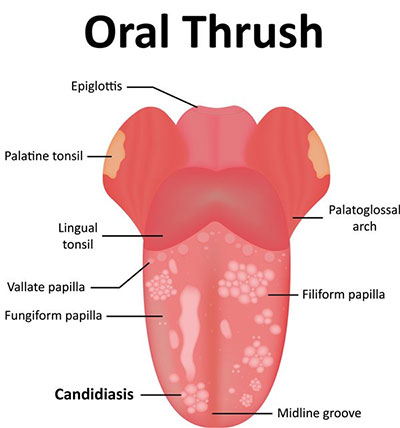
Women suffer from Candida infections four times as much as men because of hormonal factors, and are at greater risk of iron deficiency. Notwithstanding all this, the disease is also a common sign of uncontrolled diabetes. In the elderly, a major predisposing factor is the wearing of dentures. Chronic Atrophic Candidosis (generally known as denture sore mouth) may result from poor denture hygiene, and when the denture is worn on a 24-hour basis.
The infection appears as redness, with swelling of the gums, which is generally confined to the outline of the denture. When the white patches of the Candidosis are presented in adults and cannot be scraped off easily, the situation may be quiet serious. The condition can be considered to be a Candidal Leuplakia which is accepted as pre-cancerous. Frequently, dentists detect such a scenario in inveterate smokers of tobacco.
 Several easily recognised clinical entities have been identified in which Candida is at least circumstantially involved. One of them is angular cheilitis that we Guyanese call “white corner”. The victim usually complains of dryness and burning sensation at the corners of the mouth. Vitamin B deficiency often may play a role in initiating such lesions. Another case is median rhomboid glossitis. These big words simply describe the painless smooth areas we sometimes accidentally discover on our tongue. The palate opposite the lesion may also be affected.
Several easily recognised clinical entities have been identified in which Candida is at least circumstantially involved. One of them is angular cheilitis that we Guyanese call “white corner”. The victim usually complains of dryness and burning sensation at the corners of the mouth. Vitamin B deficiency often may play a role in initiating such lesions. Another case is median rhomboid glossitis. These big words simply describe the painless smooth areas we sometimes accidentally discover on our tongue. The palate opposite the lesion may also be affected.
Treatment for Candidosis must be done by one who is able to assimilate the significance of the prevailing condition as it relates to the patient as a whole. Diagnosis and treatment must be done by a competent professional. Drugs available for therapy include fluconazole, clotrimazole and nystatin.




.png)









